February is American Heart Month and Black History Month. Heart disease is the number one cause of death in the U.S. and the globe and it is mostly preventable. According to the American Heart Association, cardiovascular disease affects underrepresented groups more severely with Black/African Americans experiencing “a higher burden of risk factors” and who have twice the mortality rate of cardiovascular disease than White/Caucasian Americans.
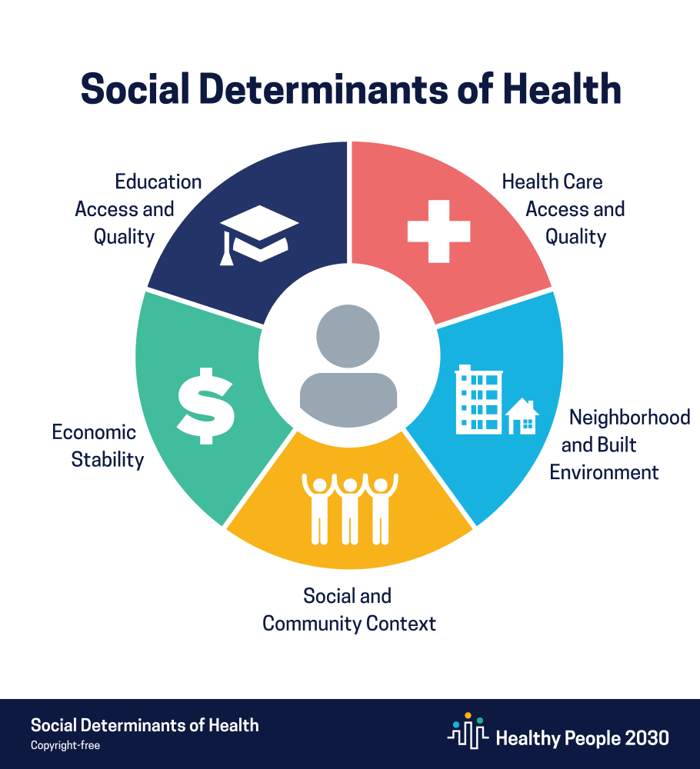
Considering that cardiovascular disease is largely preventable, we know that nutrition, lifestyle and environment are what contribute to the disease, all of which are outside the clinical context. The Office of Disease Prevention and Health Promotion outlines conditions that affect health, functioning and quality-of-life outcomes as the five social determinants of health, which include (1) economic stability; (2) education access & quality; (3) healthcare access and quality; (4) neighborhood and built environment; (5) social & community context.
Prolonged stress undoubtedly contributes to negative health outcomes including high blood pressure and diabetes, which make an individual four times more likely to develop heart disease. Evidence from reports by the American Heart Association consistently shows a positive correlation between racial discrimination and increased blood pressure. “Perceived discrimination has been associated with poor preventive health practices, such as low disease screening rates.”
According to the 2018 National Healthcare Quality and Disparities Report, hospitals in underserved communities “have higher readmission and mortality rates from cardiovascular disease.” There is a huge need to address cardiovascular issues early on before hospitalization is necessary to save lives. Better access to preventative care especially in underserved communities can go a long way. By providing high-value care through direct primary care, which re-establishes the doctor-patient relationship, patients’ health issues can be properly evaluated and treated early. There are Black/African American direct primary care doctors who are working to serve their communities and make significant contributions to changing health outcomes for the better.
Direct primary care doctors of all backgrounds can take an active approach concerning cardiovascular health by staying informed with the tools, tech, and resources available to provide the best preventative care to their patients. In the recent Tech-Docs Lunch Chat with our DPC docs, Dr. Brad Brown and Dr. David Cameron joined by Cardiologist Dr. Martin Yussman, the doctors discussed the markers and targets for monitoring potential cardiovascular disease including measuring heart rate variability and the tech available to monitor it such as Garmin and Apple Watch. The doctors also discussed calcium scores and how often one should test depending on age and risk factors and when it is appropriate to seek support from a specialist such as a cardiologist. Watch the recorded livestream for more insights.

