There are three ways self-insured employers run their health plans.
Third-party administrators (TPAs)
As the name implies, TPAs are third-party entities that handle the administrative aspects of self-funded health plans. Since they are specialized firms, TPAs have the expertise employers often do not have, to manage self-funded health insurance plans.Employers pay TPAs a fee to manage employee claims and other incidental activities. More specifically, the duties of TPAs can include:
- Plan design and drafting: Employers may work with TPAs to choose and design the benefits they offer to their employees. The TPAs may also draft the plan/policy document.
- Enrollment: TPAs usually enroll employees and manage their eligibility for the health plans. They may also educate employees on the benefits available to them.
- Claims processing: This involves scrutinizing and paying out employee claims. TPAs also sometimes provide hospital bill auditing and subrogation services.
- Compliance: TPAs ensure that the self-funded health plans are designed and operated in accordance with the Employee Retirement Income Security Act of 1974 (ERISA), the Health Insurance Portability and Accountability Act (HIPAA), the Americans with Disabilities Act (ADA) and other federal acts that self-funded health plans are subject to.
- Provider network management: TPAs choose provider networks for employers. They also secure discounts and oversee the services dispensed by providers.
- Data reporting: TPAs furnish employers with detailed information and data on claims and costs.
- Wellness program development
- ID card issuance
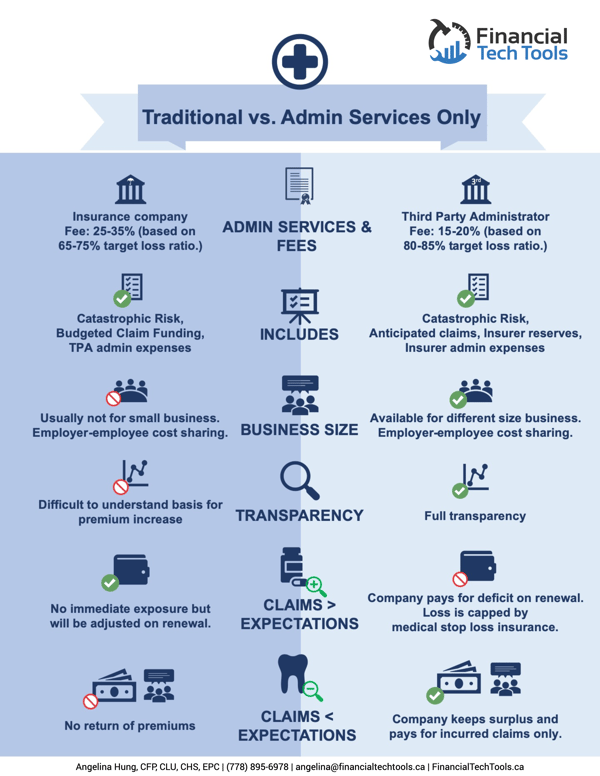
Administrative services only (ASO)
ASOs are contracts employers enter into with insurance companies to administer their self-funded health plans. In a way, an ASO is a form of TPA arrangement, except that it exclusively involves using the services of an insurance company instead of just any specialized firm’s services.Under ASOs, the insurance company, for a fee, helps the employer assess and process claims. They can also undertake any of the activities TPAs do on behalf of the employer.
Insurance companies typically have standard-form ASO agreements employers can choose from. Larger employers can, however, negotiate some of the agreement terms, or have the insurance companies create custom ones for them. The major insurers that offer ASO agreements are Blue Cross Blue Shield, UnitedHealthcare, Cigna, and Aetna. Together, these big four insurers are also known as BUCA.
Note: Insurance companies have begun taking on more ASO contracts and its become a significant revenue source for them. While they are technically only administering plans, they may seek to use similar practices as in their traditional business. It’s worth discussing an ASOs role and practices before entering into a direct contracting agreement in order to minimize interference in patient care.
You’ll discover that employers are referred to as ‘plan sponsors’. This is because, although claims are processed externally in Third-Party Administrators and Administrative Services Only arrangements, employers still bear the full financial liability for all employee claims. The employer funds claims as they are approved.
TPAs and ASO-offering insurance companies also have no contractual relationship with the employees whose claims they process.
In-house management
Some large employers have the resources to set up a department for administering the self-funded health plans. In this arrangement, all activities required to run and manage the health plans take place in-house, by designated employees.For employers, the greatest advantage of managing self-funded plans in-house is data access. Employers have access to all the data about healthcare claims, expenditure, care provider, and pharmacy costs- in any format they desire.
This data is extremely useful in fine-tuning health plans to be more cost-effective and can lead to better healthcare outcomes. Certain employers may also find that hiring staff to run the health plans is more cost-effective than paying TPA or ASO fees.
What is Stop-loss Insurance?
You may come across one other type of arrangement called ‘Stop-loss’. It’s a type of insurance product that employers can purchase to protect themselves from unexpectedly high claims. It helps to cap their risk when employee claims go over particular fixed amounts. Some TPAs offer stop-loss insurance while others that don’t, often facilitate stop-loss coverage between the employers they work with and insurance companies.Stop-loss insurance coverage is also included in ASO packages. However, some carriers that offer stop-loss insurance are reluctant to cover self-insured employers that neither use third-party administrators nor enter into ASO agreements. This is largely due to skepticism that claims will be reviewed properly in-house.
Note:It is possible for an employer to combine these different methods of self-insurance management. A third-party administrator or insurance company can manage the responsibilities that the employer is ill-equipped to take on, while the rest are handled in-house.

