It’s no secret that leaders at many healthcare organizations large and small are in full freak out mode during the COVID-19 pandemic. Seemingly overnight, the crisis obliterated demand for elective and routine care, leading to plummeting revenues. Primary care practices are no exception. In a recent study by the MGMA, primary care practices reported an average 60% drop in patient visits and 55% drop in revenues during the first three weeks of the stay-at-home order. In another study by the Primary Care Collaborative, 80% of clinicians report their practice is under “severe” or “close to severe” strain due to COVID-19. Why is this happening?
COVID-19 is not destroying medical practices. A 55 year-old business model that values quantity over quality is.
The root problem behind shrinking primary care revenues isn’t that patient visits and reimbursements are down (they are). The fundamental issue is that primary care is “reimbursed” on a fee-for-service basis to begin with. Reimbursement incentivizes quantity of care over quality of care—6-minute visits and referrals over outcomes and patient experience. Even before the pandemic, insured adults have been seeking less primary care than ever before, a trend driven by rising out-of-pocket costs and implicitly by a lack of perceived value for the money. So if your practice is suddenly struggling and you’re looking for the reason, it’s not you. It’s not COVID-19. It’s your outdated business model.
Not all primary care practices are seeing a precipitous drop in revenue.
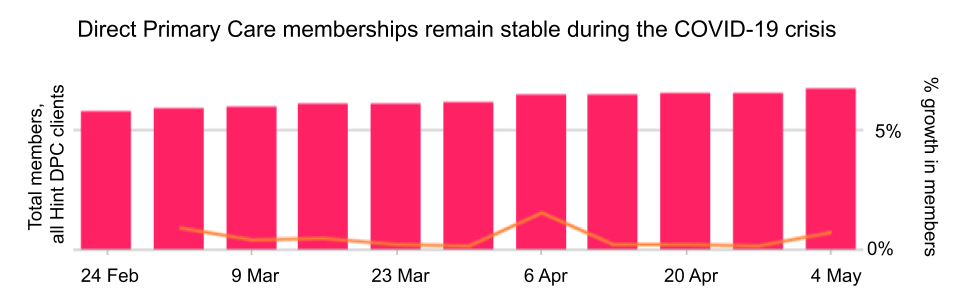
Compared to the dire financial hardships that so many fee-for-service practices are experiencing, Hint’s primary care customers are doing relatively well. That’s because our customers operate in a direct-to-consumer and direct-to-employer prospective payment model known as Direct Primary Care, or DPC. According to aggregated practice revenue data, Hint’s DPC customers averaged 1.5% growth in memberships since the onset of stay-at-home orders in mid-March.
DPC practices charge a flat recurring membership fee instead of billing insurance. These fees, typically $60-100/mo, cover services defined by the practice. With a panel of just 500 patients, a DPC physician can generate $30,000 to $50,000 in monthly recurring revenue with 20-40% lower overhead costs thanks to the absence of CPT coding, pre-authorizations, billing and reimbursement, and other administrative artifacts of the fee-for-service regime. Operating in a direct primary care model frees physicians and organizations up to focus on patient experience, health outcomes, and value.
Change is possible. We can help you pivot into a DPC model in 6 weeks.
Next Tuesday, May 12th at 7 PM ET, we’re hosting a live 1-hour informational webinar to outline a transformative 6-week program that can take you from dreaming about a better way of practicing medicine to actually doing it.
About the program
Using proven methods she’s developed over the last 10 years, you’ll be guided by veteran practice conversion expert and International Coaching Federation certified coach, Lauren Tancredi, to design your DPC offering and prepare your practice for a successful re-launch. The initial 6-week program takes the guesswork out of plan design, pricing, operations, patient agreements, marketing, sales, enrollment, membership management, and more. But that's not where our support ends. After the planning phase, we will help you launch your DPC offering and provide a 12-week program of marketing and sales support plus coaching and check-ins.
If you or someone you know is ready to leave the soul-crushing and inefficient fee-for-service system behind to practice a more liberating and more fulfilling form of medicine, join us next Tuesday at 7 PM ET to learn if our practice conversion program is a good fit for you.

