Demonstrate Value at Every Visit with Advanced Plan Administration
As a DPC provider, you are always looking for ways to reduce costs and improve patient satisfaction. Operating outside of the third party payer system allows you to offer services and procedures at cash pay prices that are steeply discounted compared to traditional fee-for-service rates. However, it's not always obvious to the patient or employer that the rate they are receiving is a far cry from what they would pay in the fee-for-service world, that's where Advanced Plan Administration can help.
In addition to these cash pay discounts, many services you provide in your clinic are included in the cost of a DPC membership. Based on a study released by the Society of Actuaries, the majority of DPC providers include office visits, telemedicine, EKGs and biopsies, to name a few, as covered services provided in the cost of a patient’s DPC membership. As a DPC provider, it is often hard to demonstrate the value the patient is receiving when there is nothing to bill for at the end of a visit. Until now…
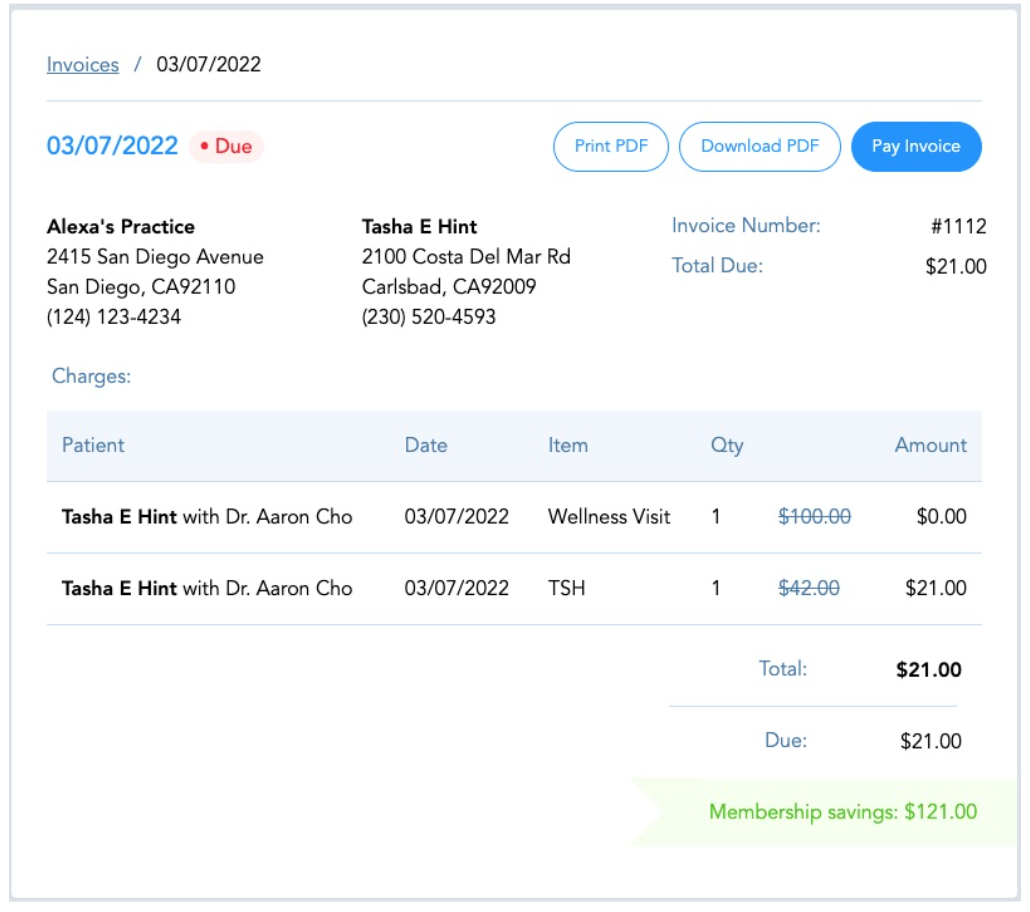
Advanced Plan Administration on Hint highlights the cash value saved at each and every visit with no additional effort from you or your team. The services included in the cost of DPC memberships and the cash pay discounts patients and employer sponsors receive calculate onto a savings banner bringing the value provided to your members front and center.
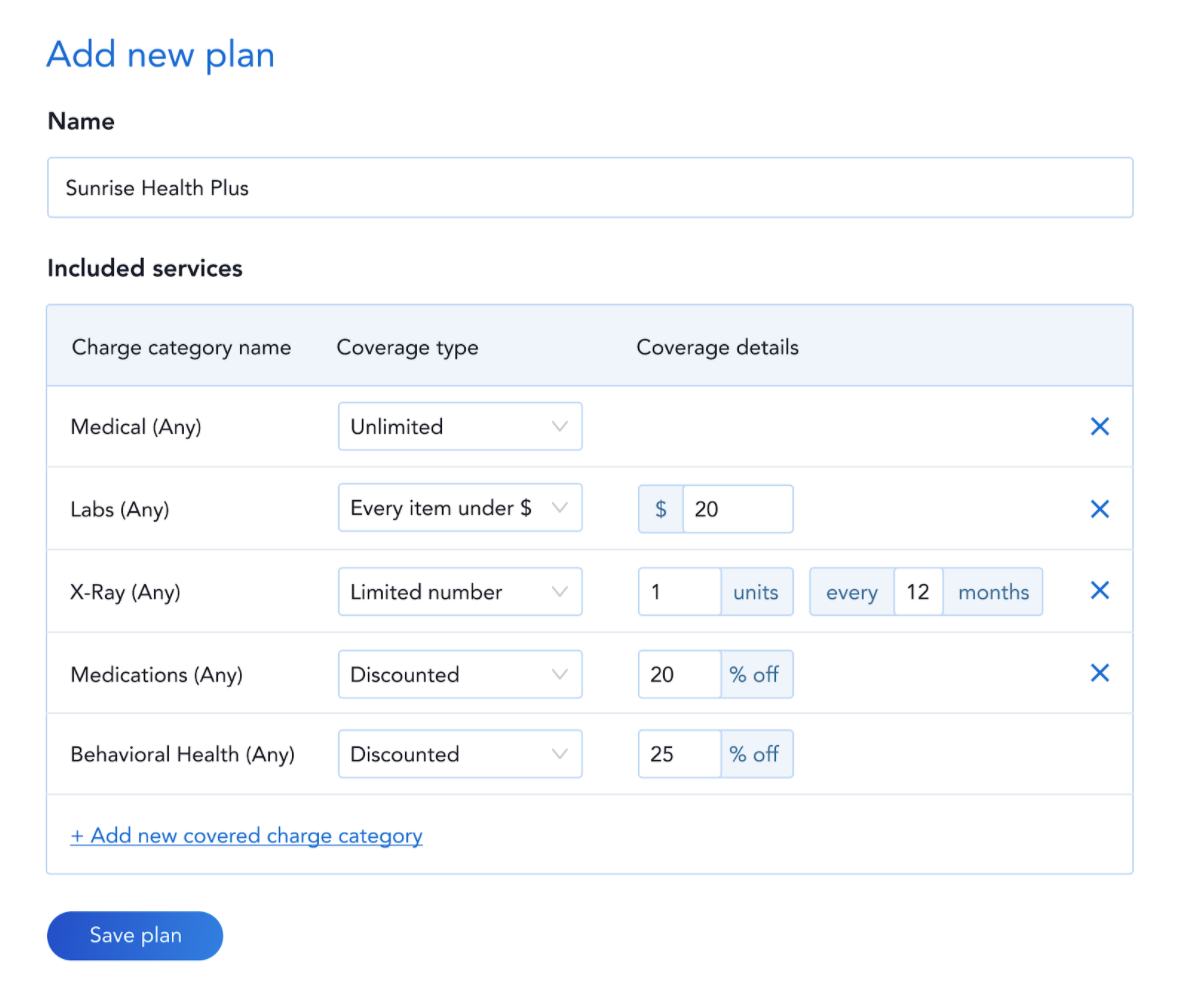
Many factors can impact what services a member is eligible to receive and who is paying for that service (patient or employer) such as membership plan tier or by tailoring the services received within each of your employer contracts. We recently connected with Primary Health Partners to learn more about their employer arrangement and learned that one of their employer groups wants to extend their coverage to pay for all labs, medications and physical therapy appointments while another group wants to cover all labs and allergy tests. This could quickly turn from a manageable operation to revenue leakage and billing errors as each patient visit is accompanied by different coverage.
Instead of having their staff refer to each member’s plan or employer sponsor every time a service is provided to determine whether or not they should create an invoice, all of their service tiers and billing rules are preset and applied to the product or service in real-time. Now having multiple coverage options does not add administrative workload, maximizing their revenue streams and possibilities for growth.
"This is [a] game-changer for us in working with some of our large employer groups. We're going to be able to drive significant savings for them just by rolling this out."
- Sharon Hodnett, VP of Operations and HR at Primary Health Partners
Automate the Intricacies of Billing
Advanced Plan Administration takes automation to a whole new level, allowing providers to set rules based on the patient’s membership plan or based on the employer sponsoring their coverage. For the services that are not included in the cost of the DPC membership, Hint automatically determines who is responsible for paying for the charge based on your preset rules and routes the charge to the appropriate party preventing billing errors and revenue leakage in real-time.
Here are just a few benefits of how Advance Plan Administration can help your practice:
√ Coverage rules based on service, product, category or price
√ Charge rules applied to invoices in real-time preventing billing errors and revenue leakage
√ Automatically route charges to the appropriate payer (patient or employer)
√ Display savings for employer sponsor and patient
√ Offer multiple service tiers without adding administrative overhead
Learn More about Advance Plan Administration here.
Interested in the Hint platform to power your direct care practice? Connect with our team.

