This article is the first in a series that examines the changing landscape of Healthcare Information Technology for Direct Primary Care. While the HIT sector has in the past been incompatible with the unique demands of running a Direct Primary Care practice, now emerging solutions are changing the landscape. In this series, we’ll look at the traditional role HIT has played in practices, the unique technological requirements of Direct Primary Care, and explain everything from Electronic Medical Records to Membership Loyalty Management. Don’t know AR from PHM? You’ve come to the right place.
Health Information Technology Focused on Insurance Billing
Information technology is a critical component of any successful business. In most industries, companies aggressively leverage technology to improve efficiency, intelligence, and reduce costs across their business. Interestingly, the US healthcare industry has been a notable exception mainly because of how providers and hospitals are paid.
For the past several decades, Health Information Technology has focused on designing solutions that help providers navigate the complexities of billing insurance because of the dominant third party payer fee for service reimbursement model. This focus has intensified in recent years driven by the passage of the $19.2 billion Health Information Technology for Economic and Clinical Health (HITECH) Act signed into law in 2009, which included the Meaningful Use program. The Meaningful Use program, coupled with new policy and payer initiatives including the Affordable Care Act, ICD-10 and revised HIPAA rules have added tremendous complexity and administrative burden on providers in their quest to successfully secure reimbursement from third party payers.
If filing for payments from Medicare and commercial insurance companies was complicated in the past, today it is nothing short of a labyrinth. As payment rules have become more complicated and burdensome, so too have the HIT systems that try to help providers navigate byzantine rules to secure reimbursement.
The (Emerging) Golden Age of Healthcare Information Technology
Thankfully, the healthcare landscape is changing driven by healthcare reform and the emergence of value based healthcare purchasing. In response, an explosion of HIT innovations hold the promise of dramatically reducing costs and improving outcomes. In addition, we’re seeing rapid adoption of EHRs driven by the Meaningful Use program, which will improve the codification and liquidity of healthcare data.
In parallel, in the private marketplace, self-funded employers are taking control of their rising healthcare spend and investing in a wide array of initiatives to accomplish “triple aim” goals - reduce costs, improve patient care experience and better manage population health. This in turn is driving into existence new value based care delivery models, such as Direct Primary Care, and HIT solutions designed to facilitate these objectives.
Finally, patients and consumers desire on-demand and cross platform HIT so contacting their providers, refilling prescriptions and follow up care are at the tip of their fingers as in most other businesses today.
Direct Primary Care & Health Information Technology
The Direct Primary Care (DPC) model was born out of a desire to restore the provider patient relationship by eliminating third party payor intermediation and the onerous requirements to obtain insurance reimbursement. Comparing the clinical, operational and economic interests between fee for service insurance and DPC highlights the fundamental differences in the care delivery models and subsequent technology needs.
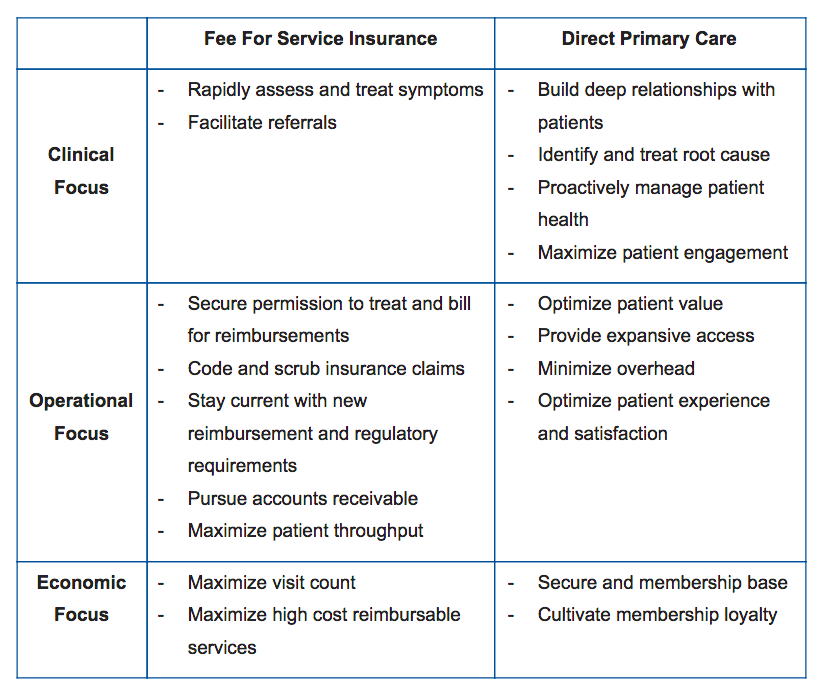
Although the overarching goal of both models is to deliver the best possible patient care, with these substantial clinical, operational and economic differences, it becomes clear that the HIT needs also differ greatly.
Fundamentally Different Purpose and HIT Needs for Direct Primary Care
The defining characteristic of DPC is the lasting and trusting relationship between the provider and the patient, which helps achieve superior health outcomes, lower costs and an enhanced patient experience. Direct Primary Care, and it’s associated supporting HIT, can accomplish this by focusing on four things:
-
Service: The hallmark of Direct Primary Care is adequate time spent between patient and physician. DPC enables unhurried interactions and frequent discussions to assess lifestyle choices and treatment decisions aimed at restoring and promoting long-term health. DPC practices have extended hours in which doctors can be reached, ready access to care, and patient panel sizes small enough to support this service commitment.
-
Replacement of Fee for Service: Direct Primary Care eliminates the perverse fee for service (FFS) incentives in primary care. These incentives distort healthcare decision-making by rewarding visit and procedure volume over value. This undermines the trust that supports the patient-provider relationship and rewards expensive and inappropriate testing, referrals and treatment. DPC replaces FFS with a simple monthly fee that covers comprehensive primary care services.
-
Medical Advocacy: Direct Primary Care providers are committed advocates for their patient members within the healthcare system. They have time to make informed, appropriate referrals and support patients when necessary outside of the primary care setting. DPC providers accept the responsibility to serve as expert healthcare navigators for their members.
-
Stewardship of Health and Healthcare Dollars: Direct Primary Care providers believe healthcare must provide more value to the patient and the system. Healthcare must be more patient-responsive, less invasive, and less expensive than it is today. The ultimate goal is health and wellbeing, not simply the treatment and management of disease.
Given that focus of the HIT industry has been squarely on supporting the fee for service model, the needs of the Direct Care model are very much under met today. But, now that we understand the core focus of the Direct Care model we can define the core technology requirements needed to support its success.
In our next post, we will provide a detailed overview of the core technologies required to support a successful Direct Primary Care practice.

